Winter is fast approaching and it won’t be long until Mother Nature visits with her annual “gifts” of snow, ice, and cold temperatures. If you are a homeowner, you know how challenging it is to stay on top of chores like keeping your sidewalks free of snow and ice, so they are safe and accessible for pedestrians. It is also important to keep stair and driveway areas clear, in order to avoid slips and falls. In this post, we will discuss some of the reasons why these types of chores are particularly challenging and what to do to avoid some of the pitfalls and injuries that occur most often in the wintertime.
Physical Challenges
Snow and ice present specific challenges to anyone living in cold climates. It is important to remove ice from walking areas, but sometimes in the very process of attempting to remove the ice, the homeowner slips and falls. In some cases, a fall might only result in a minor injury, but some people seriously injure themselves and end up with broken bones or perhaps even a concussion.
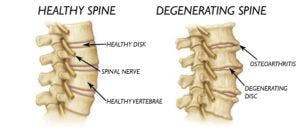
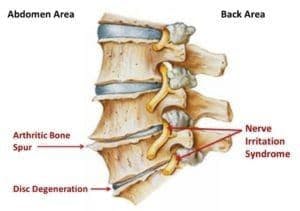
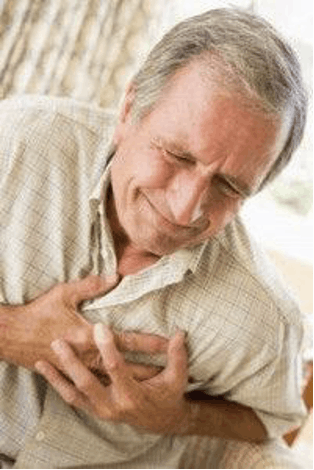
Even a few inches of snow can be extremely heavy to hoist, especially if it is wet snow. Not only is snow shoveling very challenging for those with back or knee issues, the simple physical exertion in the midst of cold temperatures can present a problem for those in poor physical condition. Cold temperatures cause blood vessels to constrict, thereby decreasing the blood supply to vital organs such as the heart. During physical movements like shoveling, the heart will beat faster demanding more blood, which is not as easily available from the constricted blood vessels. It is for this reason that physicians often call snow shoveling the “perfect storm” for heart attacks.

Be Honest About Your Abilities
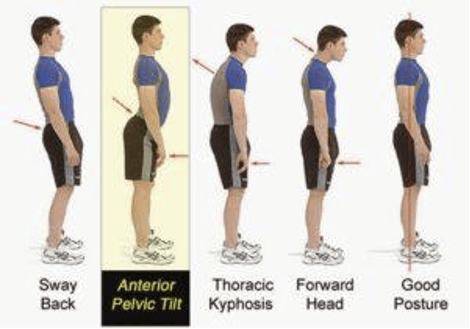
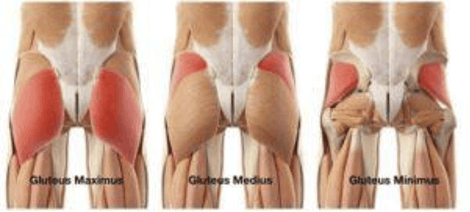
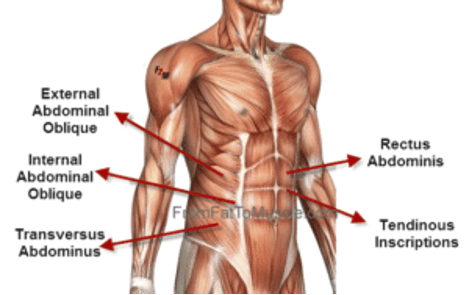
For some people, it might be time to consider if this is the year to start getting outside help for winter chores. Chores like snow shoveling and breaking up ice are challenging physical tasks. If you’ve noticed every winter it is getting more and more difficult to properly maintain your home’s exterior, or if you have physical challenges such as lumbar (lower back) pain or are prone to slips and falls, it might be time to initiate some self-care by finding alternative ways to maintain your home.
Rather than shoveling, you might want to consider investing in some snow blowing equipment if you can afford it. Most walking snow blowers are self-propelled and there are also small tractor models available that operate much like a riding lawnmower. If you don’t want to invest in any equipment or feel that even they are too strenuous to operate, do some research to find reputable companies in your area that will plow your driveway and keep your sidewalks clean. Many people maintain their independence in their own home for decades just by getting a little help with the more difficult aspects of home ownership.

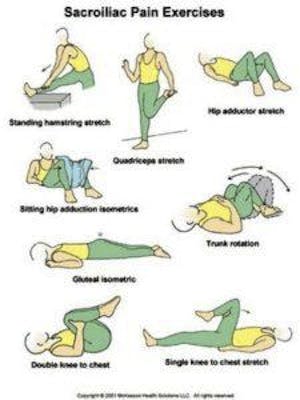
If you think you are fit enough to perform snow or ice removal chores, there are some things you can do to mitigate your chances of having a mishap. Warm up your body, just like you would do if you were going to work out. Do some stretches and jog in place for a few minutes or use a treadmill to prepare your cardiovascular system. Wear sturdy boots with good traction ability on the soles. Wear several layers of clothing rather than one bulky jacket and be sure to cover extremities like your head and your hands.
Ideally, try to get rid of any ice first so you don’t fall while trying to shovel any snow. There are many great products available that will quickly melt ice on your sidewalks, so let these types of products do the ice removal for you. If possible, try to keep up with your snow removal chores rather than letting it pile up. It is a lot easier to shovel three inches of snow rather than nine. If you have a large area to shovel, take frequent breaks, especially if the air temperature is very cold and frostbite becomes a concern. Listen to your body and don’t push it beyond its capabilities.
For more tips on how to stay safe and avoid injury during the winter season, please contact us and speak with one of our therapists to ensure your safety.
Our locations:
- Kennedy: (412)-771-1055
- Crafton: (412)-458-3445
- Allison Park: (412)-487-2787
- Bethel Park: (412) 835-2626
- Atlasburg: (724) 947-9999
Website: www.hesspt.com
Disclaimer: this information is "not medical advice" and is used at the site visitor's own risk.