Back pain can make it hard to live your life. When your back hurts, bending, moving, or even just sitting can be painful.
If you’ve got back pain, you’re not alone. An estimated 80 percent of Americans will experience a back problem in their lifetime, according to the American Chiropractic Association. There are many causes of back pain, two of which are Degenerative Disc Disease and Degenerative Joint Disease. These two conditions are similar, but there are several slight differences. Here’s what you need to know about these painful conditions, and how you can start feeling better if you’re experiencing them.

What is Degenerative Disc Disease?
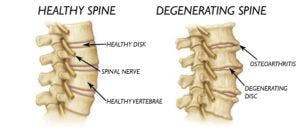
Degenerative Disc Disease (DDD) is actually not a disease. It’s a condition that affects the discs of your spine. Your spine is made up of 33 small bones called vertebrae. In between those bones are your intervertebral discs–a kind of cushion for your vertebrae made up of fibrocartilage tissue. Over time, your intervertebral discs begin to break down. Some intervertebral disc breakdown is normal due to aging. Disc breakdown can also be caused by injuries or stress on the spine. Degenerative Disc Disease occurs when your discs break down so much that it becomes painful to complete everyday tasks.
Back pain is the main symptom of DDD. This pain usually comes and goes depending on your activity level. The pain increases when you stand, walk, or lift anything. Weakness in the legs and back is another symptom of Degenerative Disc Disease.
What is Degenerative Joint Disease?
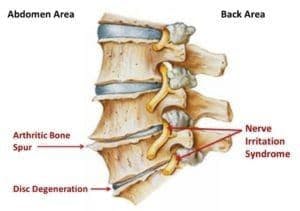
Degenerative Joint Disease (DJD) is another term for osteoarthritis–the wearing down of cartilage at the ends of your bones. This can cause your bones to rub together painfully. Osteoarthritis is the most common form of arthritis, affecting more than 30 million people in the United States. Osteoarthritis can affect joints in any part of your body, but it most commonly causes knee pain, hip pain, hand pain, and pain in the spine.
Risk factors for Degenerative Joint Disease include age and family history. Women are more likely to get DJD than men. People who are obese are also at increased risk for the condition due to the stress that extra weight puts on their joints. Symptoms of Degenerative Joint Disease include pain, stiffness in the joints, and bone spurs. DJD also often leads to poor posture.
The Differences Between DDD and DJD
The main difference between Degenerative Disc Disease and Degenerative Joint Disease is that the conditions occur in slightly different parts of the spine. DDD affects discs directly, while DJD affects the cartilage at the ends of your vertebrae. Since DJD affects other parts of the body aside from the spine, if you are also experiencing pain in other joint areas, it could be indicative of DJD. However, the two conditions can often occur together. Fortunately, both conditions can be treated in the same way.
How Can You Treat DDD and DJD?
- Pain relievers. Taking an over-the-counter pain reliever such as ibuprofen, aspirin, or naproxen sodium can often help to alleviate your back pain. If your pain is severe, your doctor may prescribe stronger pain relief.
- Supplements. Many people with Degenerative Disc Disease and Osteoarthritis take glucosamine and chondroitin–components of cartilage. However, research has shown little effect from these supplements. Recent clinical trials have shown some success with avocado and soybean oil supplements. Talk to your doctor before beginning any supplement.
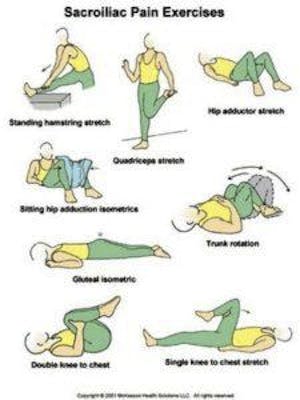
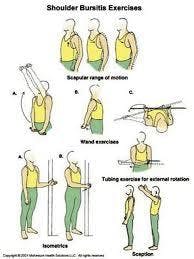
- Physical therapy. Patients with DDD and DJD can greatly benefit from physical therapy. Your physical therapist will design an individualized course of treatment. Physical therapy helps strengthen your back muscles, making movement less painful.
- Surgery. In some severe cases, surgery is considered for DDD and DJD. Surgery is only considered for patients who don’t see an improvement in their condition within three months of using more conservative methods.

If you’re experiencing back pain, Hess Physical Therapy can help! Give us a call at any of our 3 locations or refer to our website www.HessPT.com for further contact information. We can design a physical therapy plan to alleviate your pain, whether it’s caused by Degenerative Disc Disease or Degenerative Joint Disease.
Our locations:
- Kennedy: (412)-771-1055
- Crafton: (412)-458-3445
- Allison Park: (412)-487-2787
- Bethel Park: (412) 835-2626
- Atlasburg: (724) 947-9999
Website: www.hesspt.com
Disclaimer: this information is "not medical advice" and is used at the site visitor's own risk.




 [blog_locations\
[blog_locations\